From diagnosis to defiance: A doctor's battle with lupus
KUALA LUMPUR - When Dr Thipa Paneer Chelvam, 32, was diagnosed with lupus - a chronic disease that can cause inflammation and pain in any part of the body - she was in a state of denial.
"I was in denial for many years. Accepting a chronic illness into my life and making it part of me was one of my biggest challenges.
"It never occurred to me that one day I would wake up sick and never get better. At first, I was non-compliant with my medication because I thought I was okay without it,” said the psychiatrist at Serdang Hospital.
Sharing her experience in dealing with the debilitating consequences of lupus, she said, "I had frequent episodes of fever, joint pain, swollen lymph nodes, malar rash and unexplained fatigue.”
"Lupus is a mimic of other illnesses, as such I was initially diagnosed with lymphoma before my Anti-nuclear antibody (ANA) and Anti-double stranded DNA (dsDNA) became positive. Since then, I was diagnosed with lupus and was prescribed immune-suppressing tablets and steroids,” she told Bernama recently.
Dr Thipa, who completed her medical degree in Moscow, has been working as a doctor for six years. She was diagnosed with lupus, technically known as Systemic Lupus Erythematosus, (SLE) in 2015.
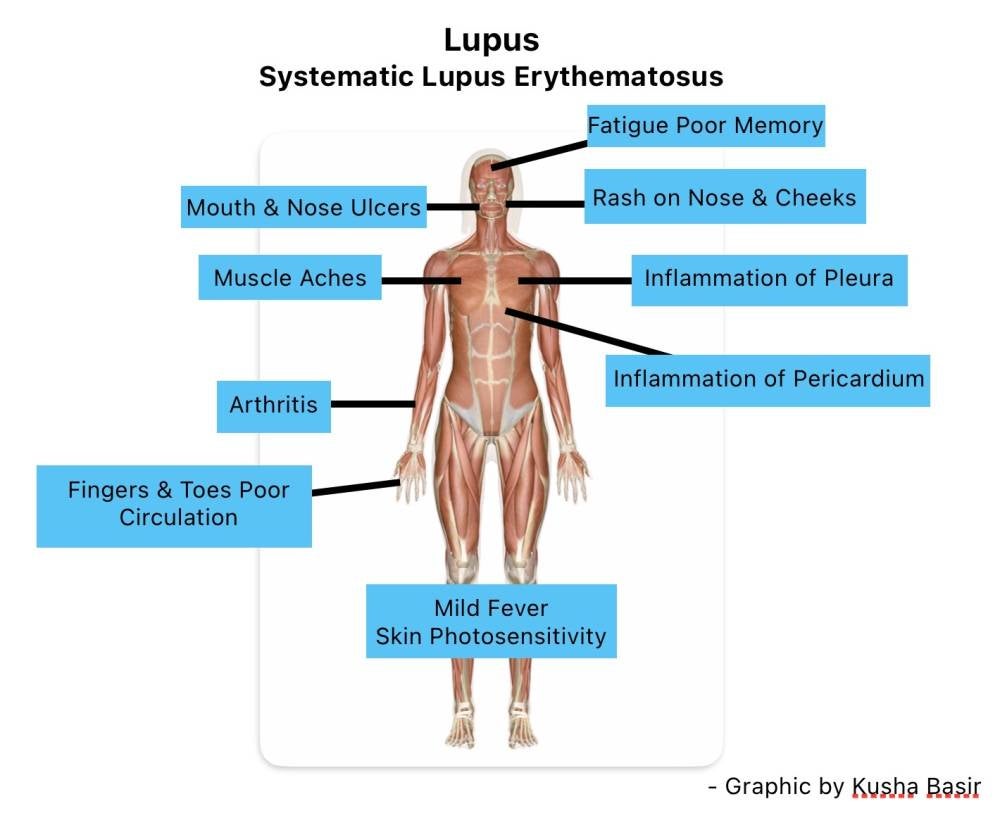
Lupus is a chronic autoimmune disease when your body’s immune system attacks your own body tissues including internal organs, which further causes organ failure and damage. This resulted in early and premature deaths.
GIVE UP OR FIGHT?
She further explained that daily steroids caused her to gain weight while immunosuppressants caused her hair to ‘fall out’ with frequent vomiting of blood.
"At that point, I wanted nothing to do with medication daily, till I realised that I had only two options medically and emotionally - to fight or to give up.
"I embraced my pain. I chose to be a lupus warrior and not a victim. I chose to fight and not quit. Ever since then, I started fighting an ugly war inside my body with a huge smile on my face.
"I think the biggest struggle I face with lupus is explaining my pain to someone who does not have a clue about my invisible illness and making someone understand that it’s a daily struggle being in pain and feeling sick on the inside when I look fine on the outside,” she said.
Living with lupus, she added, has always been frustrating as there are not are not many treatment options available.
She said, it has always been a journey of comparing her pre-lupus life to lupus life, where she is unable to expose herself under the sun, and where she feels so fragile that the slightest stress that life throws can cause a lupus flare-up.
"Living with lupus also means that I’m unable to plan things, I never know when I'll have a good day and when my symptoms will arrive. I struggle daily with brain fog and clouded memory. Living with lupus also means waking up every morning with a single desire to have a pain-free day.
"I normalised frequent admission and stay in the hospital. My constant flares and pain have many times caused me to be absent from work.
"Some days, it gets so tough that walking into the hospital, talking to my patients and just turning up is a challenge,” she said, adding that she is very passionate about creating mental health awareness in society and being an advocate for lupus including forming a support group.
WOMEN AT HIGH RISK
According to Associate Professor and Consultant Rheumatologist in the Faculty of Medicine and Health Sciences, University Malaysia Sabah, Dr Malehah Mohd Noh, generally, there are two types of lupus, one that affects only the skin (Discoid lupus) and another type that affects other internal organs of the body (Systemic lupus).
"Over 90 per cent of lupus patients are females (doctors are not sure why lupus is more common in women, but they think that differences in the genes and hormones). The majority affected are young females at childbearing years; the peak incidence in Malaysia is between 15 to 35 years of age.
"Lupus resulted from a combination of genetic and environmental factors.
"People with genetic predisposition may develop lupus when in contact with specific environment triggers, for example after a prolonged sunlight exposure or viral infection,” said Dr Malehah who is also the President of Persatuan SLE Malaysia Sabah Chapter.
As an expert in managing lupus with more than 20 years experience, her present role is to treat patients, educate medical students and the public and also conduct research in the field of rheumatology with lupus specifically.
Dr Malehah said the worldwide SLE prevalence is estimated to be 43.7 (15.87 to 108.92) per 100, 000 persons and 3.41 million people, respectively.
"Worldwide incidence and prevalence differ between countries and ethnicities. Black and Hispanics have the highest incidence while the Asian population tends to get more severe organ involvement.
"In Malaysia, we are reporting an estimation of 10,000 patients with lupus nationwide, and many more remain undiagnosed,” she added.
According to Dr Malehah, every lupus patient has slightly different symptoms from one another; some of the more common early symptoms include red skin rash shaped like a butterfly across the nose and cheeks, joint pains and swelling as well as mouth ulcers and unusual hair loss.
Besides that, warning signs include low blood counts, worsening kidney function and brain involvement like memory loss and seizures.
"There is no single test that can be used to diagnose lupus. It is often difficult to diagnose because it has many symptoms that mimic symptoms of other diseases.
"This, in turn, delays the diagnosis in most patients. Doctors use blood investigations which include a positive antibody and take complete history with a thorough examination, which subsequently concludes the diagnosis,” she said, adding that lupus can occur in children, however, it is rarely seen before the age of five and in some cases the disease starts during teenage years at an average age of 12.
CAN IT BE TREATED?
Elaborating on the matter, Dr Malehah said lupus is an unpredictable disease in which the disease activity fluctuates from time to time and this would lead patients to live their lives with uncertainty.
However, with healthy eating and lifestyle, keeping a healthy mental and physical state with good social support through family and friends, patients with lupus can lead a normal life.
"There are three different stages of lupus. First, is a flare, when it is characterised by increased disease activity. During this stage, the patient may experience worsening of symptoms or new symptoms may occur.
"A second stage called remission, refers to a period when the symptoms are minimal or absent. This can be achieved through effective treatment. Lastly, is an active stage, in which the disease remains active with recurring or persistent symptoms. Lupus is a chronic condition, where the stages may vary between patients,” she said.
Noting that there is no cure for lupus, Dr Malehah however said current medications and therapy can control the disease to allow patients to live the best possible quality of life.
"Treatment consists of immunomodulators (modulating the autoantibodies) as well as immunosuppressants (to suppress the immune system that causes damages to the internal organs). In treating an SLE patient, the doctor has to prevent flares, treat the flares, and minimise organ damage and complications.
"The common triggers for disease flare-ups include sunlight exposure, infections and stress. Which is why we always advise our patients to have adequate protection from the sun,” she said, adding that treating SLE is often a team effort between the patient and several types of healthcare professionals namely rheumatologists, nephrologists, hematologists, dermatologists, neurologists and psychiatrists.
There should also be regular communication with healthcare providers as it is pivotal in managing lupus patients effectively.
Dr Malehah opined that public awareness of lupus is significantly poor, especially among low socio-economic and education status.
She said although there has been effort to promote awareness, there are a lot of misconceptions and myths about lupus, likely because it’s a disease with poor understanding.
"Our main objectives in Persatuan SLE Malaysia are to create, increase and improve public awareness about lupus, showing support to our patients through understanding them, encouraging and motivating them. Our activities include share and care, where the patient and their family members can discuss their difficulties relating to their lives affected by lupus.
"Other activities include public awareness campaigns through radio, television and programmes to the public. Our yearly event ‘Walk-a-Payung’, is where our participants will be walking with an umbrella to show their support for lupus patients as well as a symbol of their understanding to protect them from direct sun exposure that could flare up the disease,” she added.
THE IMPORTANCE OF SUPPORT SYSTEM
Meanwhile, describing her experience with lupus as a "love-hate relationship”, Dr Thipa said, "I hate it that I had to hit rock bottom to become the best version of myself, but I also love that it was the beginning of the most amazing chapter of my life, regardless of my struggle,” she said.
Sharing her family and friends as pillars of support especially in difficult times when she was diagnosed with lupus, she also created a lupus support group in August this year.
"It has been a great journey since then, to have people who run the same race as me and to fight the same pain as me, has been a blessing. We share our pain and struggles each day and help each other through our challenges. I love my lupus warriors.
"Living with lupus can be isolating, especially when those around you might not understand what you go through daily. The most important way I manage lupus is to love myself and lupus itself. I never beat myself into my daily routine. I give my mind and body the biggest priority.
"I choose to say no to my triggers and to remove stressors that caused my flares. I practise mindfulness, meditation and deep breathing as a way to manage my daily stress. I am honest and open about my pain and struggle. Living with a chronic illness can be emotionally challenging,” she said, adding that she always surrounded herself and leaned on her support system when she could not manage emotionally and physically. - BERNAMA










